Surgical Treatments
Oral and maxillofacial surgery is known as the branch of medicine that performs surgical procedures related to teeth and the surgical treatment of pathological formations in the soft tissues of the mouth (tongue, cheeks, salivary glands, etc.). Jaw and dental problems, which can affect the most basic human functions, primarily breathing, speaking, and chewing, can be eliminated with jaw and dental surgery solutions. Dental surgery, which has the potential to significantly improve quality of life along with these functions, also provides positive aesthetic benefits to the patient.
Surgical Treatments
Contents
What is Sinus Lift Treatment?

A sinus lift is a surgical procedure performed to elevate and expand the sinus cavity. Elevating the sinus cavity may be done to prevent or treat sinus infections, or to reduce sinus pain and discomfort. A sinus lift procedure can be performed by a dentist or plastic surgeon and is usually done under local anesthesia. The sinus lift procedure may vary depending on the patient’s condition and needs and may be performed in conjunction with other surgical procedures in some cases.
In dentistry, a sinus lift is a surgical procedure used to address toothlessness in the area when there is insufficient bone tissue for implant placement. This occurs in patients who have lost their upper molars and, over time, have experienced bone resorption and downward displacement of the sinus.
How is a Sinus Lift Performed? What are the Sinus Lift Methods?
The maxillary sinus is the name given to the anatomical cavities located above the upper jaw, near our molars. The function of these cavities is to aid in sound production and reduce the weight of the skull. When the sinus cavities sag downward, bone volume loss occurs. This bone loss can be seen as a natural physiological process, but if implant treatment is planned, it can cause problems when sufficient bone height cannot be achieved. Sinus grafting is used to fill sagging sinus cavities in order to perform implant treatment in edentulous areas. If implant treatment is to be performed on a patient experiencing bone volume reduction due to sinus sagging, a sinus lift surgical procedure is performed first as part of the treatment.
If a patient experiencing bone volume loss due to sinus sagging is to undergo implant treatment, sinus lifting surgery is performed first. This procedure creates sufficient volume for the length and width of the implant, which must be fully placed into the bone. Once sufficient bone volume is achieved, the implant is placed. It is extremely important that implant treatments requiring sinus lifting are performed by maxillofacial surgeons who are experts in the field. Sinus lifting is performed under local or general anesthesia. After this operation, which lasts about half an hour, mild pain that can be relieved with painkillers may occur. After the procedure is completed, it usually takes 4-5 months for the desired bone tissue to form in the area. The sinus lift operation can be performed in two different ways depending on the thickness of the bone under the sinus.
Closed Sinus Lift
This is the protocol for placing an implant after grafting, following tooth extraction or by reaching the sinus floor through the crest apex, after elevating the sinus membrane, when there is insufficient bone height for implant placement but there is sufficient bone thickness to allow for intervention.
Open Sinus Lift
When the bone height between the crest and the sinus floor is very thin, and attempting to access the crest carries a high risk of bone fracture, a window is opened in the buccal bone surface to reach the sinus floor. The sinus membrane is then elevated, and graft material is placed.
A sinus lift can be performed under local anesthesia in the dentist’s chair. The gum tissue in the sinus area to be lifted is made accessible through a small window opened inside the mouth. After the sinus membrane covering the inside of the sinus is lifted, bone powder and grafting are performed in the created space. The area is then closed with stitches.
What are the graft materials used in sinus lifting?
In cases of bone deficiency, the materials applied to the area where bone formation is desired are called bone grafts. These bone grafts can be taken from the person’s own body (usually from the jawbone and hip bone), can be of animal origin (bovine grafts), or can be synthetically produced. Allograft materials are generally used in sinus lift treatment. Due to religious requirements in our country, bovine grafts are preferred over porcine grafts.
What Should Be Considered After a Sinus Lift?
Sinus lift surgery, also known as sinus elevation surgery, is performed to treat sinus sagging caused by missing molars. The surgery, which takes approximately 2 hours, involves filling the resulting gaps with bone powder to prevent sagging. It takes approximately six months for the bone powder to fuse with the bones. The following should be noted after the procedure:
- The tampons placed inside the mouth should be bitten down firmly for at least 45 minutes, after which ice should be applied. This should be done until bedtime.
- They should not be spat out under any circumstances, and the nose should not be blown or the mouth rinsed for at least 2 days.
- Do not bathe on the first day.
- Do not consume hot drinks or foods for at least two days.
- After sinus lift surgery, eat on the other side to protect the wound area. Do not eat or drink anything for 24 hours after the procedure.
- Care should be taken when cleaning the nose to avoid applying pressure. The mouth should be kept open when sneezing.
- Smoking after sinus lift surgery can cause gum problems during the healing period. Patients should especially avoid smoking during the healing period. The operation is more successful in patients who do not smoke than in those who do.
Will There Be Swelling After Sinus Lift Surgery?
The formation of swelling varies from person to person depending on the swelling in the cheek. A cold compress can be applied for 24 hours to prevent swelling. Mild swelling in the area is normal and necessary for healing.
What is the Cost of a Sinus Lift Surgery? What Factors Affect Pricing?
The number of teeth to be implanted, the amount of bone that needs to be removed, and consequently the amount of graft material to be used, as well as the quality and size of the membrane material, affect the price of the surgery. For more detailed information, you can visit our clinic and get examined.
Tooth Extraction
Tooth extraction is a dental procedure that involves completely removing an infected, damaged, or otherwise problematic tooth from the mouth. Tooth extraction is usually necessary due to reasons such as infection, decay, gum disease, or damage caused by trauma.
Tooth extraction is generally a last resort for dentists. It is performed when a tooth cannot be saved with a filling or root canal treatment. In other words, tooth extraction is a treatment method used after all other possibilities have been exhausted.
Gum disease can cause deep pockets around the teeth and gum recession. Tooth extraction may be necessary when there is insufficient tooth structure to hold the tooth in place.
Tooth extraction may be necessary for many different reasons, including severe damage or decay. One of the most common dental procedures, tooth extraction can eliminate bacteria and improve overall oral health. Chronic bad breath caused by poor oral hygiene due to tooth decay may also disappear after tooth extraction.
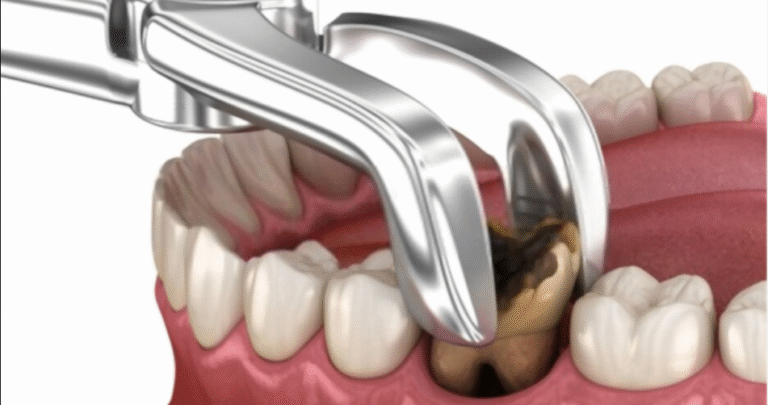
How is a Tooth Extraction Performed?
Tooth extraction can be classified as simple tooth extraction and surgical tooth extraction. In simple tooth extraction, local anesthesia is applied to numb the area around the tooth to be extracted. This ensures that only pressure is felt during the procedure. There is no pain or discomfort. The tooth is then loosened and removed using forceps. Surgical tooth extraction is usually performed when the tooth is impacted or broken at the gum line. First, local anesthesia is administered to eliminate any pain or discomfort during the procedure. The tooth is loosened using special instruments and removed from its socket. In some cases, a small incision in the gum may be necessary to remove an impacted wisdom tooth or a broken tooth. After the tooth is removed, the socket is cleaned and disinfected. In some cases, the dentist may place a bone graft to help prevent bone loss in the jaw. Finally, the incision is closed with stitches to complete the procedure.
Why Does a Tooth Break During Extraction?
One of the complications that may occur during tooth extraction is the fracture of the tooth being extracted. If there is advanced decay or bone loss in the tooth to be extracted, there is a possibility of fracture during extraction. It is important that the fractured piece is removed along with the fractured tooth. Depending on the position of the fracture, the piece can be removed using specific instruments, cut if necessary, or lifted out from the bone socket. If the broken piece remains inside after the tooth extraction, it is detected by X-ray and must be removed by re-administering anesthesia to the patient. Otherwise, over time, a cystic structure may form around the remaining piece, causing pain or jaw problems in the area.
What Should Be Done After a Tooth Extraction?
After a tooth extraction, care should be taken to rest and keep the head upright to prevent possible bleeding. Hot foods and drinks should not be consumed until the effects of the anesthesia wear off. This is very important. Because the effects of anesthesia may prevent you from feeling pain properly, you may burn your mouth. You should also be careful not to chew on your cheek without realizing it. When lying down on the first night, your head should be supported with an extra pillow and kept as high as possible. For the first 24 hours, avoid any movements that could interfere with the healing of the socket where the tooth was extracted. During this time, do not rinse your mouth, eat on that side of your mouth, or touch the extraction site with your tongue, as this could damage the blood clot. Doing so could lead to infection in the socket and negatively affect the healing process. Alcohol should not be consumed for at least 24 hours, as it may promote bleeding and delay healing. Similarly, smoking should be avoided as much as possible. Smoking after tooth extraction may increase the risk of infection and, in addition, may harm the healing process. Aspirin and similar blood-thinning medications that may increase bleeding should be avoided.
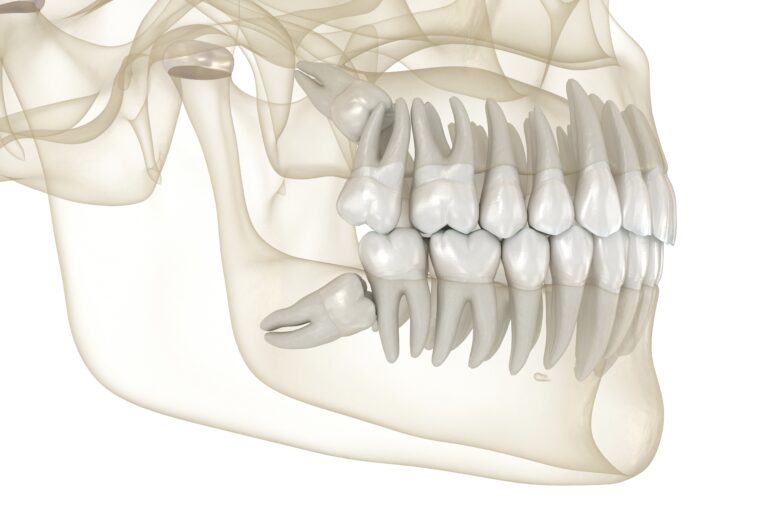
Extraction of an Impacted Wisdom Tooth
Wisdom teeth are the third molars that erupt last. They usually begin to appear in the mouth between the ages of 17 and 25. Wisdom teeth may be retained in the mouth depending on their eruption, their position when they erupt, and whether or not they cause damage to surrounding tissues. Due to crowding in the dental arch, they may remain buried under the gum tissue or completely within the bone. It is beneficial to extract wisdom teeth that are impacted.
When Should Wisdom Teeth Be Extracted?
- When there is a cyst-like formation around the tooth,
- When plaque accumulation is a source of bacteria and bad breath due to the position of the tooth,
- When there is a risk of increasing crowding in individuals undergoing orthodontic treatment,
- When there is decay or abscess formation in the affected tooth (in cases where root canal treatment is not possible),
- When the tooth is not fully erupted in the affected area and remains under the gum, causing food accumulation and gum inflammation,
- When it puts pressure on the front teeth and causes crowding,
- Problem wisdom teeth are removed from the mouth in cases of full-mouth prosthesis planning.
How Are Wisdom Teeth Extracted?
Firstly, it varies depending on the position and impaction of the tooth. In areas where the tooth is not impacted and is easily accessible, there is no difference between tooth extraction and normal extraction. After a simple extraction, there may be slight swelling, pain and bleeding. Some complex extractions requiring more specialised procedures may also be performed. After these complex extractions, swelling may increase; in such cases, antibiotics and painkillers may be used. In older age, extraction becomes more difficult and healing slows down because the bone structure becomes denser and less flexible.
What Should Be Done After a Wisdom Tooth Extraction?
Whether they cause problems or not, impacted or semi-impacted wisdom teeth should be extracted. For individuals aged 40 and above, the operation and subsequent wound healing become more difficult.
- After extraction, the gauze should be bitten down on firmly for 30 minutes; this stops the bleeding and promotes clot formation.
- The extraction site should not be disturbed, as this may cause pain, infection or bleeding.
- Do not spit. Otherwise, bleeding may increase and the clot may dislodge.
- Nothing should be eaten or drunk until the anaesthetic wears off.
- On the first day, eating and drinking should be done on the opposite side of the extraction site.
- Smoking and alcohol consumption should be avoided throughout the day.
- If the extraction was difficult, applying a cold gauze pad to the area slows circulation and prevents facial swelling.
- The application should be as follows: 20 minutes of cold compress – 20 minutes break – repeat 20 minutes of cold compress in cycles. Due to the anaesthetic effect, it may not be noticeable that the cold compress is damaging the skin. Therefore, taking breaks should not be forgotten.
- Medications prescribed by prescription should be used as directed and regularly.
Dental Injuries
Dental trauma involves trauma to the tooth as well as soft tissues such as the gums, tongue, and lips. This type of trauma can occur as a result of falls, traffic accidents, childhood play accidents, sports injuries, or blows to the face. Dentoalveolar trauma involves many tissues and structures. The tooth consists of three hard tissues: enamel, dentine, and cementum. It is attached to the tooth and alveolar bone or gum connective tissue by Sharpey’s fibres. Traumatic forces on the teeth or periodontium can cause damage in various directions and of varying degrees. Traumatic injuries are classified according to various types of fractures and luxations, but most often these injuries occur in combination.

What should I do if my tooth is completely knocked out as a result of an impact?
In this situation, urgent action must be taken. Every minute counts. It is important for parents and teachers to be knowledgeable and attentive in this situation, which is particularly common in children, and to know how to respond urgently. Information is obtained from the patient or accompanying person about when, where and how the trauma occurred. When treating teeth that have suffered trauma, it is important to record the time of the accident and the date of treatment, as this information may affect the prognosis.
When the periodontal membrane of an avulsed tooth is still viable, immediate replantation, i.e. reinsertion, is performed. It is important that this is done within 45 minutes of avulsion. If the tooth is preserved in milk or a storage solution, it can be reinserted within 24 hours.
An avulsed tooth can be preserved in milk, inside the mouth, or in storage solutions. After the avulsed tooth is brought to the clinic, it is kept in physiological saline. An oral and dental examination is performed, the patient’s history is taken, and a radiographic examination is conducted to assess the condition around the alveolar bone. For a heavily contaminated tooth, washing with physiological saline is performed to remove only the contaminants. Blood clots in the alveolar socket are washed away. The avulsed tooth is gently placed into the socket and splinted. If the adaptation between the replanted tooth and the gingiva is poor, sutures are placed in the gingiva to ensure a tight adaptation between the gingiva and the cervical region. Traditional adhesive resins and an orthodontic bent wire are used for splinting. Excessively tight splinting should be avoided as constant pressure may affect the success of the replanted tooth.
In teeth with closed root tips, endodontic treatment should be started before the splint is removed (1-2 weeks after replantation). In teeth with open root tips, however, it is necessary to wait until pulp necrosis is confirmed, as revascularisation of the pulp tissue may occur.
The splint is removed after 2-3 weeks. Following the initial treatment of avulsed teeth with necrotic pulp, once apical closure has been achieved, a final, leak-proof root canal filling is performed.
What Should You Do When a Baby Tooth Falls Out Due to an Impact?
In cases of trauma to the deciduous dentition, the most important factor is the possibility of damage to the permanent tooth bud that will replace it. The patient’s age, the malposition of the deciduous teeth, and the direction and force of the impact are some of the factors involved. Trauma to the deciduous teeth may lead to discolouration and enamel hypoplasia, anatomical crown and root curvature and malformation, and root hypoplasia in the permanent teeth. It is important to inform the patient’s family about the possibilities and to resolve any issues during the replacement of the deciduous teeth with permanent teeth. Periodic check-ups are mandatory. Enamel hypoplasia can be restored after the tooth erupts. Crown and root curvature can be treated with orthodontic and restorative procedures.
A Small Piece of My Tooth Has Broken Off. How Can It Be Treated?
If the fracture is small, polishing or selective grinding may be performed; larger fractures are restored with composite resin filling. If the broken piece is present, it can be bonded back into place. If it is not present, it can be restored with composite material.
What should be done if a tooth is both broken and loose as a result of an impact?
Crown fracture associated with luxation Firstly, restorative treatment should be performed according to current standard procedures. If no vital response is obtained from the pulp after a few months, root canal treatment should be performed. In many cases where pulp necrosis is observed following traumatic injury in young patients, the first option is to achieve apicalisation. However, in teeth where root development is fully complete, endodontic treatment followed by restorative treatment should be performed.
Jaw Cysts
Cysts can appear anywhere in the human body; however, they are most commonly seen in the jaw. Cysts settle in the soft tissue or bone inside the jaw, contain fluid, are surrounded by tissue, and grow in the area where they are located. Cysts that form in the jaw are a pathological condition. As they are detected by radiology, they may sometimes not show symptoms such as swelling and pain, and may be seen by the dentist during routine dental check-ups. Cysts are treated surgically. Cysts that form in the jaw can be removed by a jaw surgeon through surgery. If not treated in time, they can cause inflammation in the facial area, deform the jawbone, or lead to benign or malignant tumours. Dental cysts, which are fluid-filled sacs that develop in the jawbone and soft tissue, are known to be the second most common type of odontogenic, or tooth-derived, cysts. They form on unerupted teeth, partially erupted teeth, and most commonly on molars or canine teeth. Although benign, if left untreated, they can cause complications such as infection. Although dental cysts are generally benign, they are defined as anomalies that require treatment due to their size, location, and potential to cause infection.

What Causes Dental Cysts?
Dental cysts usually form at the tips of the roots of dead or dying teeth. They typically arise due to fluid accumulation on teeth that have not yet erupted. Odontogenic tumours and cysts usually originate from tissues and cells involved in normal tooth development. Most are closely linked to genetic syndromes. Individuals with nevoid basal cell carcinoma do not have the gene responsible for suppressing tumours in their bodies. Consequently, there is a risk of multiple odontogenic cysts developing within the jaw.
What Risks Can a Dental Cyst Pose?
Even a small dental cyst should be removed to prevent future complications. If left untreated:
Infection: An infected dental cyst can cause periodontal and periapical infections.
Tooth loss: An untreated dental cyst can cause problems in the gum tissue, weakening it and leading to the loss of the tooth’s ability to remain in place.
Jaw fracture: When the jawbone is weakened due to any dental cyst infection, there is a risk of fracture. The risk is higher when the cyst is located in the premolar region.
Ameloblastoma or jaw tumour: These are rare tumours that primarily affect the jaw near the molars or wisdom teeth. Jaw tumours arising from the cells that form the enamel layer can become cancerous if left untreated and may spread to the lungs or lymph nodes.
Is it possible to leave dental cysts untreated?
Although the exact causes of jaw cysts are generally unknown, they are commonly found in the jaw or in areas of the mouth close to the teeth. While most are benign tumours that do not cause any problems, they can grow rapidly over time. When problems such as growth occur, discomfort may be felt and the cyst may progress towards the sinus cavity. It is recommended that they be removed before they become malignant. While those that do not grow or cause discomfort do not require treatment, those that cause discomfort are more often removed under general anaesthesia. The decision to leave them in place should be made after evaluating the location, condition, and other factors of the tumour.
How Are Jaw Cysts Diagnosed?
What is a cyst? A cyst is essentially a pathological cavity. It expands from the centre to the periphery, becomes surrounded by a soft membrane, and fills with fluid. Treating jaw cysts is very important; if left untreated, cysts grow progressively and can lead to the loss of adjacent teeth and even fracture of the jawbone. They are mostly diagnosed by radiology. Swelling and, rarely, pain may occur in the area where the cyst is located. Cysts can be diagnosed by radiology, but sometimes they may not show any symptoms; in this case, they are diagnosed during dental examinations. Pathological examination is required for diagnosis after surgery.
How Are Jaw Cysts Treated?
Jaw cysts are structures that form in the bone and soft tissues of the jaw region and are usually filled with fluid. These cysts continue to grow and cause pain if they become inflamed. Jaw cysts, which present with symptoms such as numbness in the lower lip and palpable swelling, are identified using imaging techniques. Jaw cysts are treated surgically. The enucleation method used in surgery is applied in the treatment of smaller cysts. With this method, the entire cyst is removed in one go. The marsupialisation method is applied for larger cysts that cannot be removed in one go. In this method, a drain is first inserted into the cyst to reduce its size, and then it is completely removed. Both methods are performed under general or local anaesthesia. If dental cysts have an abnormal pathogenic structure and cannot be cured with medication, surgical removal becomes necessary. When planning cyst surgery, the location, size, and symptoms caused by the cyst are comprehensively evaluated.
What is the Recovery Process Like After Cyst Surgery?
Following the dentist’s advice and taking prescribed medication regularly is crucial for a swift recovery after dental cyst surgery. Due to their negative effects on the healing process, alcohol and smoking are not recommended after the operation. Alcohol can thin the blood and reduce the amount of oxygen in the blood, delaying the healing process. Smoking also negatively affects tissue healing and increases the risk of infection. Teeth should not be brushed and mouthwash should not be used until the doctor gives permission. Otherwise, there is a risk of bleeding in wounds that have not yet fully healed.
Apical Resection - Root Tip Removal
The pulp chamber, a cavity within the tooth, contains the pulp, which is the living tissue (nerves, blood vessels, and connective tissue) that keeps the tooth alive. A root canal system branches off from this chamber. Endodontic treatment, commonly known as root canal treatment, is required when the pulp becomes inflamed or infected. This becomes necessary in cases of deep tooth decay, repeated dental procedures on the tooth (e.g., replacing a large filling), or traumatic damage such as cracks or even fractures. If the pulp dies, the pulp chamber and canals can become infected. This infection can eventually spread to the surrounding bone and other tissues at the tip of the root. To perform root canal treatment, a hole is drilled into the tooth, and the inflamed or infected tissue is removed from the pulp chamber and root canals. The cavity is disinfected, filled, and sealed. However, in some cases, root canal treatment may not be possible, or the treated root canals may become reinfected. In such cases, apical resection becomes a treatment option.
Apicoectomy is an endodontic procedure involving the removal of the root tip, the creation of a root-tip cavity, and its filling with a special root-tip filling material.
Apicoectomy, also known as root-end resection, is a surgical endodontic procedure typically performed after a root canal procedure has failed. Root canal treatment treats infected tissue inside the tooth by removing the dental pulp and filling the tooth with gutta-percha, a biocompatible material. Although this procedure is usually successful, infected debris may remain in the tooth canals and lead to infections in the future. A patient whose tooth becomes reinfected after root canal treatment may experience pain, sensitivity, or swelling in the gums. However, some patients may not experience any symptoms. Apicoectomy removes the root tip, called the apex, and the infected tissue to completely eliminate the infection and restore the tooth to a healthy state. The root tip is where nerves and blood vessels enter the tooth and then pass through the canals to reach the pulp chamber. Removing the root tip ensures that the infected tissue at the source of the problem is eliminated, leaving no infected tissue in the tooth.
In Which Cases is Apical Resection Performed?
- When conventional root canal treatment fails
- When infection develops after root canal treatment
- When repeated root canal treatment is unlikely to be successful
- When conventional root canal treatment is not indicated
- It may be performed for various anatomical, pathological, and traumatic reasons.
How is an Apical Resection Surgery Performed?
Before commencing apical resection surgery, local anaesthesia is administered to numb the area. A small incision is then made in the gum tissue at the level of the affected root. This provides direct access to the infected periapical tissues. The infected tissue near or around the root tip, along with the last few millimetres of the root tip, is removed. A very small filling is placed at the end of the root canal to seal it and prevent further infection. The gum tissue is closed with small stitches. Where necessary, particularly if the infection has caused a significant cavity, bone grafting and other techniques are used to aid bone growth.

What happens if apical resection is not performed?
If apical resection is not performed, infection and swelling may occur in the tooth roots. If infection and swelling occur, apical resection is necessary. Otherwise, there is a risk of experiencing significant pain and discomfort.
What Should Be Considered After Apical Resection?
It is normal to experience some pain after apical resection. Painkillers prescribed by the dentist can be used to control the pain. Mild bleeding may occur in the first few days after apical resection. During this process, you should avoid spitting, smoking and using straws. This will prevent the necessary and protective blood clots in the surgical area from dislodging. Swelling may be seen for the first few days following apical resection. This swelling usually resolves on its own within 1 week. Ice compresses should be applied for the first 12 hours after apical resection surgery. To prevent irritation of the surgical site, consumption of hard and crunchy foods should be avoided for a few days. Patients can usually return to their daily routine a few days after apical resection surgery.
Tooth Abscess
A dental abscess can be described as a localised collection of pus in the alveolar bone at the root tip of a tooth or the structures supporting the tooth (e.g. the gums). It is a bacterial infection that can affect both children and adults and may be painful or painless. Dental abscesses can occur in both chronic and acute forms and are generally categorised according to their location: periapical abscess, gingival abscess, and periodontal abscess. Although dental abscesses are usually localised in the affected tooth or supporting structures, the pus formation often spreads to nearby tissues, leading to serious complications.
A collection of pus caused by a bacterial infection in the tooth or gums is called a dental abscess. There are different types of dental abscesses that can occur in different areas of the tooth for various reasons. A periapical abscess occurs at the root tip of the tooth, called the apex, a periodontal abscess occurs where the gums meet the teeth, and a gingival abscess occurs in the gums.

What are the symptoms of a tooth abscess?
- Pain
- Abscess
- Swelling and redness in the gums or face
- Bad taste or odour in the mouth
- Fever
- Sensitivity in the teeth to hot and cold food and drink
- Swelling of the lymph nodes in the neck area
- Difficulty swallowing or opening the mouth
- Swelling in the lower or upper jaw may indicate a serious infection.
How is a Tooth Abscess Treated?
Dental abscess treatment is planned on an individual basis with the aim of curing the infection, preventing complications and, if possible, saving the tooth. The treatment to be applied depends on the extent of the problem. At this stage, the condition of the abscessed tooth and whether the infection has spread to other teeth is determined by taking a dental X-ray. Incision and drainage: A small incision is made in the abscess to drain the pus. After the pus is drained and the swelling subsides, the abscessed area is cleaned. Root canal treatment may be required after the abscess is drained. Root canal treatment: This is an effective dental procedure that eliminates the infection and saves the tooth. After the infected pulp of the tooth is removed, the resulting cavity is filled to prevent a new infection. Although the pulp is very important during the growth of the tooth, mature teeth can survive without pulp after the necessary treatments are performed. After root canal treatment, the tooth may need to be crowned. Tooth Extraction: Tooth extraction may be necessary when it is not possible to save an abscessed tooth. When the tooth is extracted, the pus in the area drains out. The area is thoroughly cleaned and disinfected. Implant treatment may be an effective solution to replace the missing tooth. Antibiotic treatment: Antibiotic treatment may be considered in cases where the infection has spread and the patient’s immune system is weak. The use of antibiotics is not recommended for the treatment of dental abscesses.
What Happens if a Tooth Abscess is Left Untreated?
If a tooth abscess is left untreated, the infection can spread throughout the body, leading to extremely serious health problems. Teeth and gums are as important to the body as any other organ. Neglecting oral health needs can adversely affect overall health. If the bacteria causing the tooth abscess enter the bloodstream from the infected tooth, various health problems can arise. The body’s response to attack by bacteria and viruses can vary. The first target of bacteria is the bones, including the jawbone. Bone infection, or osteomyelitis, is inflammation that occurs in the bone marrow or bone due to a bacterial infection passing through the bloodstream. Severe cases of osteomyelitis are very painful and can damage bone structure. The most dangerous situation is when bacteria take over the body and pose a life-threatening risk.
What is cavernous sinus thrombosis?
Cavernous Sinus Thrombosis is a rare and potentially life-threatening condition in which an infection originating in the eyes, ears, nose, or teeth spreads through the blood vessels around the face, triggering more serious conditions. Parapharyngeal abscess; an infection that occurs in the deep part of the neck, causing swelling of the infected area and potentially blocking the airway, leading to difficulty breathing. The most serious condition that can result from an untreated dental abscess is considered to be sepsis. It occurs when a bacterial infection spreads throughout the bloodstream and triggers inflammation that damages organs and can block arteries. When there is insufficient blood in the body, blood pressure drops and the kidneys, liver and lungs fail due to septic shock. As many medical conditions related to the spread of bacteria in the blood can lead to sepsis, dental abscesses should not be taken lightly.
What are the ways to prevent gum abscesses?
To prevent gum abscesses, it is essential to maintain healthy teeth and gums. Routine dental check-ups should not be neglected, and teeth should be cleaned regularly. Teeth should be brushed twice a day with fluoride toothpaste. Dental floss should be used regularly to clean the areas between the teeth and gums that are difficult to reach with a toothbrush. The consumption of sugary foods and drinks should be limited. Otherwise, you may be faced with cavities that can lead to abscesses.
Preprosthetic Surgery
If a prosthesis is required but there are ongoing issues such as gum recession or jawbone atrophy, pre-prosthetic surgical procedures may be necessary. Pre-prosthetic surgery refers to any type of oral or maxillofacial surgery that helps prepare the patient’s mouth for a dental restoration. Treatment may involve rebuilding areas of bone loss or smoothing the gums and alveolar ridge, depending on the individual patient’s needs. The primary aim of pre-prosthetic surgery is to ensure that the dentures fit comfortably and securely in the patient’s smile and function fully.
All treatment procedures performed to prepare the patient’s mouth prior to prosthesis placement are referred to as pre-prosthetic surgery. Pre-prosthetic oral and maxillofacial surgery consists of a series of procedures performed to prepare the patient for full or partial prosthesis applications. In some patients, minor oral surgical procedures are required before partial or full dentures can be fitted to ensure maximum comfort. As dentures rest on the bone ridge, it is very important that the bone is of the appropriate shape and size. When tooth extraction is necessary, the underlying bone may be sharp and irregular. In this case, the bone may need to be smoothed or reshaped to ensure the best possible fit for the denture. In some cases, excess bone may need to be removed before the denture can be fitted.
Who is Preprosthetic Surgery Performed On?
The patient’s suitability for pre-prosthetic surgical procedures is determined during the prosthetic consultation. The need for such procedures is determined based on the shape and contours of the patient’s mouth, particularly the alveolar ridge and gums. In cases of abnormal bone development, the denture may fit loosely. In addition, food and bacteria can accumulate more easily under dentures that do not fit properly. This can increase the risk of gum disease and chronic bad breath. Furthermore, the denture may not be able to perform its functions properly. Individuals who experience jawbone recession following tooth loss or who have excess gum tissue that hinders restoration may require surgery prior to prosthesis placement.
When is Preprosthetic Surgery Performed?
The goal of pre-prosthetic surgery is to prepare the soft and hard tissues of the jaw for a comfortable prosthesis that will restore oral function, aesthetics, and facial form. Pre-prosthetic surgery aims to provide comfortable and effective solutions for the following conditions:
Restoration of jaw function (chewing, swallowing and speaking)
Preservation or improvement of jaw structure
Enhancement of facial aesthetics
Elimination of pain and discomfort caused by an ill-fitting prosthesis as a result of surgical alteration of the area where the prosthesis will be placed
Improvement of the area where the prosthesis will be placed in patients with significant alveolar bone loss
Placement of endosseous implants in the jaw
Improvement of the condition of excess bone ridges or overlying soft tissues prior to prosthesis fabrication to ensure prosthesis retention and stability.
What are the types of preprosthetic surgery?
Preprosthetic surgery refers to the preparation of the mouth prior to the placement of dental prostheses such as removable dentures or implants. For prostheses to rest on the gums covering the bony ridge of the jaw and fit comfortably and properly in the mouth, the bone ridge must be smooth. As the structure of the mouth varies from person to person, prosthetic applications may not proceed smoothly in the same way for every patient. In such cases, prostheses may slip, wounds may form in the mouth, or prostheses may be fitted incorrectly. Therefore, in necessary situations, different pre-prosthetic surgical procedures may be performed to reduce the bone ridge, soften and reshape the bone, and remove excess soft tissue or bone.
Alveoplasty: The upper and lower jawbones consist of two different types of bone: the alveolar bone, which surrounds the teeth, and the basal bone, which forms the dense foundation supporting the alveolar bone. Following tooth extraction, irregular areas often develop in the alveolar bone during the healing process. Due to these irregular areas, prosthetic applications can cause significant pain and instability. Therefore, prior to prosthetic applications, a procedure called alveoplasty may be used to smooth and reshape poorly or irregularly healed alveolar bone. Alveoplasty can be applied to a small area or a more general region. The degree of alveoplasty required usually determines the most appropriate type of anaesthesia for the procedure. As part of the alveoplasty procedure, an incision is made in the gum tissue over the irregular areas. The bone in the area is then smoothed, the bone ridge is reduced, and the bone is reshaped to best fit the planned prosthesis. The area is closed with stitches to complete the procedure.
Excess Bone Removal (Torus Removal): Abnormal bone growth in the mouth is not unusual and generally does not cause concern. Generally completely harmless, toruses, which are excessively large bone formations, typically appear in two specific areas: the hard palate, known as the Torus Palatinus, and the area under the tongue in the lower jawbone, known as the Lingual Torus. These bone formations, seen in approximately 9% of the population, are not generally considered a major problem except for individuals who frequently traumatise the area or patients planning to have dentures fitted to replace missing teeth. Dentures significantly traumatise the bone areas where toruses form and lead to poor denture retention. Minor growths do not always need to be removed. However, moderate to large irregularities can seriously affect the fit of dentures. Exostoses located on the outer edge of the alveolar ridge and touching the cheeks, torus on the lower alveolar ridge touching the tongue, or torus on the hard palate must be removed. Excess bone on the hard palate may interfere with upper dentures or cause speech impediments. A small incision is made in the gum tissue to remove the excess bone. Bone formation is reduced and corrected using special instruments. After creating a smooth and flowing form from the treated upper or lower jaw, the area is closed with stitches.
Removal of Excess Gum Tissue (Gingivectomy):
Vestibuloplasty: Vestibuloplasty is generally a procedure performed only on the lower jaw and only on the front part of the lower jaw. In patients who have been missing teeth for some time, the body responds by breaking down and resorbing the bone in the areas where teeth are missing. If this occurs in the front of the lower jaw, atrophy and resorption can cause the remaining bone and gum tissue to be too low to support a prosthesis. As a result, vestibuloplasty may be performed to lower the muscle attachments of the lower lip to the appropriate area of the lower jaw and increase functional height. This allows the soft tissue to be extended to a position where sufficient support for the prosthesis can be obtained from the existing bone.
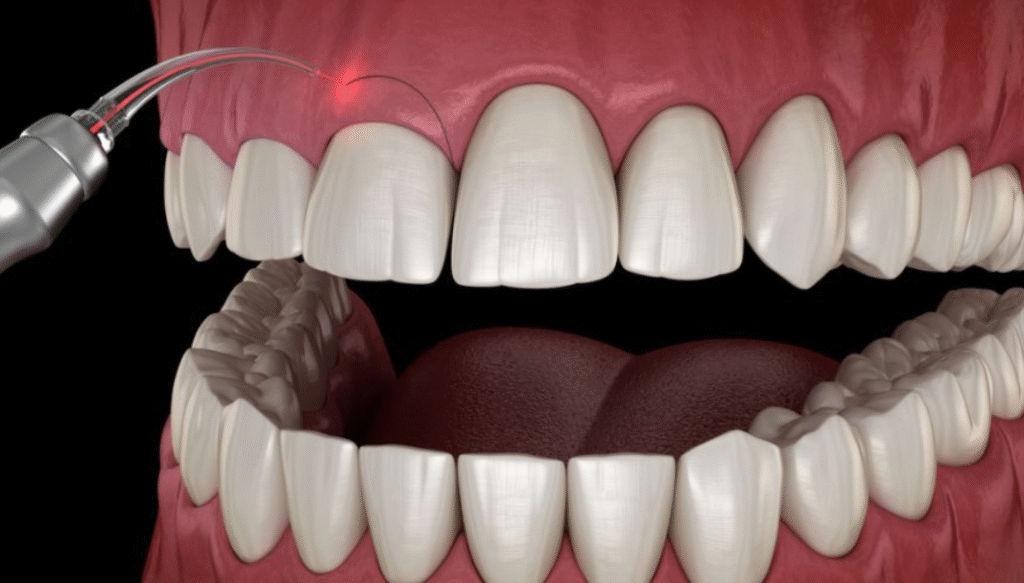
Frenectomy: The frenulum refers to a normal anatomical muscle attachment area between the upper and lower lips and the upper and lower jaws, and between the underside of the tongue and the back of the lower jaw, known as the lingual frenulum. The frenulum varies in characteristics from person to person. The lingual frenulum is a collection of tissue under the tongue that causes ankyloglossia or ‘tongue tie’. This condition is characterised by restricted movement of the tip of the tongue due to a short or large lingual frenulum. Frenectomy is an extremely simple procedure in which excess frenulum tissue is cut and, in some cases, removed. It is performed to allow the surrounding tissues to move and function more appropriately.
Exposure of Impacted Teeth: Certain conditions, such as severely misaligned teeth, can prevent dentures from fitting properly. Impacted teeth that have not fully erupted are also among the factors affecting the fit of the restoration. In such cases, tooth extraction may be required before dentures can be fitted. While some extractions are straightforward, complex surgical techniques may be required for the extraction of impacted teeth.
What are the Risks of Preprosthetic Surgery?
Although advanced techniques and technology used today have reduced the likelihood of complications, there are still some risks associated with pre-prosthetic surgery. Potential problems include infection, excessive bleeding, bone necrosis, unwanted tissue growth, allergic reactions, scarring, nerve damage, bone graft rejection, and bone resorption in cases of bone augmentation. Choosing a qualified surgeon is the most effective way to reduce potential risks.
What is the Recovery Process Like After Preprosthetic Surgery?
Recovery after pre-prosthetic surgery largely depends on the type and extent of the procedure performed. Some inflammation and swelling are common after most treatments. Anti-inflammatory medication prescribed by the doctor should be taken regularly during this phase. If an incision was made during the procedure, ensure that gentle tooth brushing and flossing techniques are used near the surgical site. Depending on the type of surgery, it may be possible to return to work the next day, although this may vary depending on the individual patient. Care should be taken to rest in order to ensure a quick and healthy recovery process. The duration of full recovery may vary depending on the scope of the procedure. When gum excision is performed, recovery is usually complete after about a week. If a bone ridge augmentation procedure has been performed, recovery can take 6 to 9 months.
How Should One Eat After Preprosthetic Surgery?
Following pre-prosthetic surgery, the doctor may recommend a special diet during the recovery process. As healing progresses, the diet can be gradually expanded to include soft foods. Popcorn, nuts, foods containing small pieces, and spices may irritate the gums during this process. Therefore, these types of foods should be avoided for several weeks.
What are the Advantages of Preprosthetic Surgery?
Preprosthetic surgery significantly improves the fit and function of prostheses. Secure prostheses can also improve a person’s systemic health. When prostheses fit correctly, a more complete diet, rich in all the nutrients the body needs, can be implemented. Pre-prosthetic surgery can enhance a person’s appearance, giving them a more youthful look. Prostheses that fit perfectly become indistinguishable from natural teeth. Furthermore, the contours and proportions of the smile can be improved by softening the gum line and alveolar ridge.
Is tooth extraction painful?
Tooth extraction is normally a painful process. However, the dentist administers local anaesthesia beforehand to ensure that no pain is felt during the extraction. This means that the patient only feels pressure during the extraction. There is no question of feeling pain or discomfort. It is normal to experience a certain level of pain after tooth extraction. The pain that may occur after tooth extraction can be controlled by using simple painkillers prescribed by your dentist.
Is pain after a tooth extraction normal? How long does it last?
Pain may occur for a period of 1 to 3 days after tooth extraction. If sensitivity is high, pain may be felt for up to a week. In this case, using painkillers prescribed by the dentist may be effective.
What should I eat after having a tooth extracted?
After tooth extraction, alcohol and hot food and drinks should not be consumed for at least 24 hours. For one week after tooth extraction, hard, crunchy and chewy foods such as crisps, nuts and popcorn should not be consumed. In addition, as chewing tough pieces of meat may be difficult, they should not be included in the diet.
Can you smoke after having a tooth extracted?
Smoking is not recommended for the first 3 days after a tooth extraction. Smoking after a tooth extraction can delay the healing process and cause inflammation. Blood clots at the site of the tooth extraction are important for healing. Smoking can cause the blood clots to dislodge, delaying the healing process.
Can I drink alcohol after having a tooth extracted?
Alcohol should not be consumed for at least 72 hours after tooth extraction. It is recommended to avoid alcohol for 7 to 10 days to allow the extraction site to heal completely and for the blood clot to form properly.
Is an abscessed tooth extracted?
In cases where extraction is the best way to eliminate infection, an abscessed tooth may be extracted. The method used to treat infection in the nerves, roots, or surrounding gum tissue of the tooth may vary depending on the location and extent of the infection. In cases of infection, there is a risk that bacteria in the mouth may reach the pulp and cause nerve damage. In such cases, the tooth should be extracted to prevent such damage. If the damage is not excessive, root canal treatment may also be a solution. In this procedure, after the infection is drained, the area is sealed to prevent bacteria from causing reinfection.
How many teeth can be extracted in one go?
It is not possible to specify a standard number of teeth that can be extracted in a single session. This can be determined based on the patient’s needs, general health, oral health, the condition and location of the teeth to be extracted, and similar factors.
What is alveolitis? When does it occur?
The name given to the bone section that carries the alveolar teeth. Inflammation of this bone is called alveolitis. Alveolitis is also known as dry socket. After tooth extraction, the socket where the tooth roots were seated is exposed and a blood clot forms on it. The formation of a blood clot is the first stage of healing. The blood clot that protects the nerve endings in the tooth socket may sometimes fail to form for various reasons or may be lost during the healing phase due to contamination from food debris or smoking. In this case, a condition called dry socket or alveolitis may occur. One of the current approaches to treating alveolitis is the application of PRF. In this method, a fibrin layer formed from white blood cells obtained from the patient’s own blood is placed in the extraction socket. This allows the inflamed alveolar bone to heal quickly.
What should be done after a tooth extraction?
Under normal circumstances, routine oral care can be resumed 24 hours after a tooth extraction. However, teeth should be brushed gently, paying special attention to the extraction site. Toothpaste or water should not be forced out. If only liquid nutrition is being consumed, dental floss may not be used for the first few days following the extraction. Using dental floss aggressively near the extraction site may cause unnecessary inflammation.
Where do cysts occur?
Dental cysts usually occur around the roots of dead or infected teeth, around impacted wisdom teeth, in the gums, or in the jawbone.
Can the formation of dental cysts be prevented?
Dental cysts rarely develop around living teeth. If the nerves in a tooth die as a result of infection or trauma, the tooth should be treated as soon as possible to prevent it from becoming a source of infection. The tissues next to the root should not be stimulated to form cysts or abscesses, so regular visits to the dentist are essential. If the patient is suspected of having an impacted tooth, more detailed examinations can detect dental cysts while they are still small, and cyst formation can be prevented by removing the potential starting point.
Do cystic lesions need to be treated?
If cystic lesions in the teeth are left untreated, pain may develop over time. In addition, problems such as root resorption, the cyst destroying the surrounding bone as it grows, and causing thinning of the bone due to pressure may occur. Thinning of the bone can lead to fractures in the jawbone. Furthermore, depending on the location of the dental cyst, the patient may experience problems such as jaw spasms and difficulty opening the jaw.
Can't dental cysts be treated with antibiotics?
Treatment of small dental cysts may involve the use of antibiotics or anti-inflammatory drugs.
What is done during cyst surgery?
The technique to be used during cyst surgery should be determined on a case-by-case basis according to the type of dental cyst. Depending on the size of the cyst, it may be preferable to insert a drain in necessary cases, reduce the size of the cysts first, and then remove them through surgical procedures. The type of anaesthesia to be used should also be determined by assessing the size of the cyst and the general health status of the patients.
Why is surgery performed before prosthetics?
The most suitable time for performing pre-prosthetic surgery is either at the same time as tooth extraction or at least 6 weeks prior to the measurement and formation stage of the prosthetic process. The area where the surgical procedure is performed requires at least 6 weeks to heal. This ensures the most accurate results in terms of prosthesis production. Complete bone healing cannot be achieved until approximately 12 weeks after surgery.
What is bone graft?
One of the procedures used to increase bone volume in areas where bone volume is low is bone grafting. Bone graft material can be used as a ready-made material or can be harvested from the patient’s oral tissue or other body areas. When the jawbone has lost its function or is insufficient, bone grafting is performed with the aim of restoring the jawbone to a quality, adequacy and strength suitable for implant placement.
What are the risks of bone graft application?
All surgical procedures currently in use carry risks such as bleeding, infection and anaesthetic reactions. During bone grafting, there is also a possibility of encountering risks such as pain, oedema, nerve injury, bone graft rejection, inflammation and graft resorption.
Does bone loss affect teeth?
Bone loss affects all bones in the body, including the jawbones. Loss of bone density in the jaw compromises tooth stability, increasing the risk of tooth loss and periodontal disease. Bone loss affects both natural teeth and dental implants. Osteoporosis, or bone loss, significantly increases the risk of periodontal disease by weakening the bones.
Is an implant performed on a person with bone loss?
Although implant treatment is not recommended for patients with osteoporosis, the decision should be made on a case-by-case basis. Factors such as the rate of bone loss, Z-score, T-score, the patient’s general health status and age should be taken into consideration. In cases where advanced investigations are required, tests such as CTX, NTX, and alkaline phosphatase may be necessary. Implants cannot be placed in osteoporosis patients who receive bisphosphonate-containing drugs intravenously. Good bone quality is essential for successful implant treatment. Problems may arise with the retention of implants placed in areas where bone quality is reduced. This can lead to undesirable situations such as implant loss. To prevent such situations, dentists may prefer to increase bone quality by compressing the area where the procedure will be performed using a device called an osteotome.
What can be done if an implant is not possible?
Dental implants not only look like natural teeth and perform the same functions, but also play a significant role in preventing jawbone loss. However, every patient is unique, and dental implants may not be the best choice for every individual. They may be contraindicated for medical reasons or may not be preferred by the patient. Full dentures, partial dentures, and fixed bridges are treatment alternatives that can be used in cases where implants are not performed.
Who cannot have implants?
Implant treatment cannot be performed on individuals who use intravenous bisphosphonates, whose general health condition prevents implant treatment, whose jawbone structure is unsuitable for implants, who smoke heavily, who have uncontrolled systemic diseases, who have a teeth-grinding habit, or who have advanced bone loss or gum disease.
If there is no bone, can an implant be placed?
In cases where there is insufficient bone in the area where dental implant treatment will be performed, a bone grafting procedure should be used and sufficient bone should be obtained using different techniques. One of the methods that can be preferred for this is to place bone taken from the patient themselves or artificial bone tissue in the area of the jaw where the procedure will be performed. In addition, bones scraped from another area of the patient’s jaw where there is bone can be applied to the area where there is no bone, and artificially prepared bones can also be applied to the area where the implant will be performed.
